Aims: The addition of tyrosine kinase inhibitors (TKIs) has significantly improved the prognosis of Ph-positive (Ph+) B-cell acute lymphoblastic leukemia (B-ALL). However, there are still a certain proportion of patients resistant to conventional means or relapse after treatment. In current study, the efficacy and safety of CAR-T bridging to allo-HSCT for patients with relapsed/refractory (r/r) Ph+ B-ALL were evaluated.
Methods: Between November 2018 and July 2023, 29 consecutive patients with r/r Ph+ B-ALL were included. The median age was 32(2-61) years old, 17 male and 12 female. All patients were not in CR MRD-(complete remission with negative BCR/ABL fusion genes detected by real-time PCR)status, 11 cases in CR MRD+ and 18 cases in NR (not remission). 10 patients had clear extramedullary lesions. 15 patients had mutations in the coding region of the ABL1 gene T315I kinase. 9 patients had a history of allo-HSCT.
After CART treatment, the patient sequentially enters the transplant procedure. 5 patients received allo-HSCT from sibling HLA matched donors, 19 patients from haploidentical donors and 5 patients from unrelated donors. Myeloablative conditioning regimens with total body irradiation (fractionated, total 10 Gy) /etoposide (200mg/m 2 x 3) /fludarabine (30mg/m 2 x 5) or cyclophosphamide (1.8g/m 2 x 2) /rabbit anti-T-cell globulin were used. The infusion count of MNC cells was 4.35-15.36×10 8/kg and CD34+ cells was 2.57-8.5×10 6/kg. Cyclosporine, mycophenolate mofetil and short-term methotrexate were employed for graft-versus-host disease (GVHD) prophylaxis. All patients received sensitive TKIs up to 2 years post-transplantation.
Results:
After CART therapy, 7 of the 11 patients with CR MRD+ status obtained CR MRD-, and 4 still in CR MRD+. 11 of 18 patients with NR status obtained CR MRD-, 6 patients obtained CR MRD+ , and 1 case still in NR.
In the allo-HSCT procedure, all patients achieved durable engraftment. 5 patients developed mild aGVHD, 4 patients developed severe aGVHD, 1 patient developed mild cGVHD, and 6 patients developed severe cGVHD. All of them were resolved with immune-suppressants except 1 patient died. CMV reactivation occurred in 14 patients and EBV reactivation in 1 patient. 6 patients developed hemorrhagic cystitis. 14 patients developed definite organ infections, of which 11 were pulmonary infections, the others were intestinal infections, perianal infections, urinary tract infections, and sepsis. 5 patients were infected by the COVID-19 virus during epidemic, and 1 of them progressed to pneumonia.
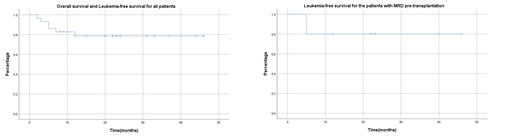
The median follow-up time was 21 (2-46) months, 23 patients are alive to date, of which 22 patients have no leukemia and 1 patient has recurrent molecular MRD and still receiving treatment. The 2 years overall survival (OS) and leukemia-free survival (LFS) both reached 78.6% (95%CI 0.583-0.898). Among the 6 deceased patients, 1 patient with pre-HSCT NR did not achieve remission after transplantation and died of severe aGVHD, 2 patients died of recurrent leukemia after transplantation, and 3 patients died of severe infection. The non-relapse mortality (NRM) was 13.8% (4/29).
After treatment, of the 10 patients with extramedullary lesions, 8 (8/10) were living without leukemia. Among the 15 patients with ABL1 gene T315I kinase region mutation, 13 (13/15) were leukemia-free survival. Of the 9 patients with a history of allo-HSCT, 6 (6/9) survived without leukemia. Among the 10 patients with pre-transplantation CR MRD+ status, 8 (8/10) were leukemia-free after transplantation, the 2 years LFS was 80% (95%CI 0.527-0.869).
Conclusion: Our results indicate that CAR-T bridging to allo-HSCT is safe and effective for patients with r/r ph+ ALL. The 2 years OS and LFS both reach to 78.6%. The risks associated with treatment are acceptable. Even for patients with extramedullary lesions, patients with mutations in the T315I kinase region of ABL1 gene, and patients with a history of allo-HSCT, good results can be achieved, indicating that CART bridging to allo-HSCT appear to overcome above adverse prognostic factors. Although a proportion of Ph+ALL patients (this proportion seems to be higher than Ph-ALL) still can not achieve CR MRD- after CART treatment, this does not prevent patients from transplantation carrying MRD and achieving good results (2 years LFS is 80%). Therefore, in clinical practice, if it is very difficult for patients to obtain CR MRD-, allo-HSCT is also recommended.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal